Interesting articles
9 Signs of alert on ovarian cysts that women ignore women
Detecting ovarian cysts premium is important for your treatment, but sometimes give symptoms that are overlooked. Let's see what they are.
At present, a large part of the female population is affected by the disease or polycystic ovarian syndrome. This means that in your ovaries there are numerous cysts, which are usually harmless and various sizes.
It is a small bags filled with liquid that are located inside or on the surface of the ovaries. Its main cause is hormonal decontrols and are usually developed at any age during reproductive years.
Although they do not represent a serious health problem, it is important to detect them in a timely manner to prevent them from continuing to grow.
For this a series of physical symptoms should be taken into account that, although they can indicate other conditions, they could also be keys in their detection.
1. Changes in urination
Changes in urination habits are a signal that allows you to detect several problems in health.
If you suddenly feel more desire to urinate, and you can not even control it, keep it very into account because you can be due to ovarian cysts.
These symptoms, as well as burning after urinating, indicate that the pelvic floor muscles are weakened or infected.
In case you persist for more than two days, the most convenient is to consult the doctor to receive a timely diagnosis.
2. Abnormal bleeding
One of the most obvious symptoms of hormonal disorders are the bleeding that occur in dates away from menstruation.
Although it is common that some experience something that again, suffer it frequently should be a reason to visit the gynecologist.
3. Pain during intercourse
Vaginal infections and inflammation are usually the reason why a certain pain occurs when maintaining sex.
But if this happens to be so frequent that it even affects sex life, you should visit the specialist to study other possibilities.
4. Vomiting and nausea
Vomiting and nausea are not an exclusive symptom of women who are pregnant. Due to the hormonal imbalance that occurs by the cysts, some also suffer from continuously.
5. Abdominal inflammation
This is one of the symptoms that are most ignored because it is usually triggered by different factors.
Distitance or inflammation of the abdominal area is quite annoying and sometimes can be accompanied by pain.
suffer it recurrently and not find relief in a matter of days is a sign that indicates that something is not quite well.
6. Low back pain
A sensation of tension or pain in the lumbar zone does not always indicate a muscle problem. Sometimes its cause requires a little more analysis, since it can be a kidney infection or a disorder of the reproductive apparatus.
7. Loss or sudden weight gain
Losing weight Suddenly may seem like a blessing for those who suffer from overweight or obesity. However, if the pertinent efforts are not being made to achieve it, it is best to be careful because something may be wrong.
Something similar happens when there is a significant increase in kilos, although it takes a balanced diet and other healthy habits.
The feeling loss of appetite or too much anxiety for eating are signs that should be taken into account as symptoms of possible diseases.
8. Constant fatigue
Stress, routine and bad nutrition are the factors that further affect the constant episodes of fatigue. However, before hormonal imbalances, it also usually occurs continuously and chronically.
Feeling without energies, tired and with concentration problems are sufficient signals to consider this problem.
9. Pelvic pain
Pelvic pain is a very important sign of polycystic ovarian syndrome. If it occurs alien to the menstrual period should be a reason to consult.
All symptoms cited here can be given differently according to the case. Sometimes they are also accompanied by changes in intestinal habits and sudden mood changes.
So that no type of complication occurs, it is best to follow and request medical examinations in case it is pertinent.
Policistic ovary syndrome
The polycystic ovary syndrome (SOP) is a disease in which a woman has an imbalance of female sex hormones. This can cause changes in the menstrual cycle, cysts in the ovaries, difficulty get pregnant and other health problems.
Causes
The polycystic ovary syndrome is linked to changes in hormonal levels that hinder ovaries the release of fully developed (mature) ovules. The reasons for these changes are not clear. The affected hormones are:
estrogen and progesterone, female hormones that help you a woman's ovaries to free ovules.
Androgens, a male hormone found in small quantities in women.
Normally, one or more ovules are released during the menstrual cycle of a woman, which is known as ovulation. In most cases, the release of ovules occurs approximately two weeks after the initiation of the menstrual cycle.
In the polycystic ovary syndrome, mature ovules are not released. Instead, remain in the ovaries surrounded by a small amount of liquid. There may be many of them. However, not all women who suffer this condition will have ovaries with this aspect.
These problems with the release of ovules can contribute to sterility. The other symptoms of this disorder are due to hormonal imbalances.
Most of the time, the polycystic ovary syndrome is diagnosed in women at 20 or 30 years. However, it can also affect adolescent girls. Symptoms often start when you start the periods of a girl. Women with this disorder often have a mother or sister with similar symptoms.
What is the climacterium?
Climacteric is a transition period that lasts for years, before and after menopause, as a consequence of ovarian depletion, associated with a decrease in estrogen production1 and that loses with the years the capacity to produce hormones, Follicles and oocytes. In women, it is usually confused with menopause, which is the last menstruation. During the climacteric, the chain of processes that, from the month following puberty, have prepared the woman for pregnancy. Towards the beginning of the climacter, all ovarian follicles have already been used and the hormones that regulate the monthly cycle are not produced. In many cases, the menstrual cycle is increasingly prolonged.
What is endometriosis?
Endometriosis occurs when a tissue, like the one that covers the interior of the uterus (endometrium), grows out of the uterus, usually on the organs of the organs in the areas of the pelvis and the abdomen, in places where it is not supposed that grows.
The word endometriosis comes from the word & ldquo; endometrio “ - & ldquo; Endo “ it means & ldquo; in “ Y & LDQUO; METRIO “ means & ldquo; mother “ Health professionals call the tissue that covers the interior of the uterus (where a pregnant woman leads to her baby) the endometrium.
Health professionals call the areas of endometriosis by different names such as implants, injuries or nodules.
In what places outside the uterus, endometriosis grows?
Most times the endometriosis is in the pelvic cavity:
About or under the ovaries
behind the uterus
on the tissues that hold the uterus in place
on the intestines or the bladder
En casos sumamente raros, las áreas con endometriosis pueden crecer en los pulmones o en otras partes del cuerpo.
¿Cuáles son los síntomas de la endometriosis?
Uno de los síntomas más comunes de la endometriosis es el dolor, en su mayor parte en el abdomen, la parte inferior de la espalda y las áreas pélvicas. La intensidad de dolor que siente una mujer no está relacionada con la cantidad de endometriosis que tiene. Algunas mujeres no sienten dolor a pesar de que su endometriosis es extensiva, es decir, que las áreas afectadas son grandes o que hay cicatrización. Por otra parte, otras mujeres tienen dolores severos a pesar de que solamente tienen pequeñas áreas con endometriosis.
Los síntomas generales de la endometriosis pueden incluir (pero no están limitados a):
Cólicos menstruales sumamente dolorosos
(o incapacitantes), el dolor puede empeorar con el tiempo
Dolor crónico de la pelvis (incluye dolor en la parte inferior de la espalda y dolor pélvico)
Dolor durante o después de tener relaciones sexuales
Dolor intestinal
Períodos menstruales con sangrados fuertes
Sangrado premenstrual o entre los períodos
Infertilidad
Además, las mujeres con un diagnóstico de endometriosis pueden tener síntomas gastrointestinales que parecen un problema intestinal, como también fatiga.
¿A quién le da endometriosis?
La endometriosis puede afligir a cualquier mujer que menstrúe, desde el momento del primer período hasta la menopausia, sin tomar en cuenta que haya tenido hijos o no, su raza o su grupo étnico, o su situación económica. La endometriosis en algunos casos continúa después de la menopausia; o las hormonas que se usan para los síntomas de la menopausia pueden causar que continúen los síntomas de la endometriosis.
Los cálculos actuales indican que el número de mujeres con endometriosis fluctúa entre el 2 y el 10 por ciento de las mujeres en la edad reproductiva. Es importante tomar nota de que estos son sólo estimados y que esas estadísticas pueden variar considerablemente.
¿Si tengo endometriosis significa que no soy fértil o que no voy a poder tener hijos?
Alrededor de un 30 a un 40 por ciento de las mujeres con endometriosis no son fértiles, lo que hace que la endometriosis sea una de las tres causas principales de infertilidad en la mujer. Algunas mujeres no descubren que tienen endometriosis hasta que tienen dificultad en salir embarazadas.
Si tiene endometriosis y quiere salir embarazada, su profesional de la salud le puede sugerir que tenga sexo sin protección por seis meses a un año antes de recurrir a un tratamiento para la endometriosis.
La relación entre la endometriosis y la infertilidad es un área importante de las investigaciones. Algunos estudios sugieren que la enfermedad puede cambiar al útero de manera que no acepta al embrión. Otras investigaciones examinan si la endometriosis cambia al huevo o si la endometriosis interfiere en la manera en que se mueve el huevo fertilizado hacia el útero.
Causas de la Endometriosis
No se conoce la causa exacta de la endometriosis. Por el momento hay varias teorías que tratan de explicar la enfermedad.
La endometriosis puede resultar de algo llamado “flujo menstrual retrógrado”, en el cual parte del tejido que la mujer desprende durante su período fluye dentro de su pelvis. Mientras que la mayoría de las mujeres que menstrúan tiene un poco de flujo menstrual retrógrado, no todas tienen endometriosis. Los investigadores están tratando de descubrir que otros factores pueden causar que el tejido crezca en algunas mujeres, pero no en otras.
Otra teoría de la causa de la endometriosis involucra los genes. Esta enfermedad puede ser heredada o puede resultar de errores genéticos que hacen que algunas mujeres sean más susceptibles que otras de desarrollar esta enfermedad. Si los investigadores pueden encontrar un gen o genes específicos relacionados a la endometriosis en algunas mujeres, pruebas genéticas pueden ayudar a los profesionales de la salud a detectar la endometriosis más temprano o hasta prevenir que ocurra.
Los investigadores también están examinando la posibilidad de otras causas.
Parece que el estrógeno, una hormona involucrada en el ciclo reproductivo femenino, promueve el crecimiento de la endometriosis. Por lo tanto, algunos estudios están investigando a la endometriosis como una enfermedad del sistema endocrino, el sistema de las glándulas, hormonas y otras secreciones del cuerpo. O puede ser que el sistema inmunológico de la mujer no elimina el fluido menstrual de la cavidad pélvica adecuadamente, o que los químicos producidos por las áreas con endometriosis pueden irritar o promover el crecimiento en más áreas. Por lo tanto, otros investigadores están estudiando el papel del sistema inmunológico en estimular o en reaccionar a la endometriosis.
Otras investigaciones se concentran en determinar si agentes ambientales, como el estar expuesta a químicos sintetizados por el hombre, causan la endometriosis.
Estudios adicionales tratan de comprender que factores, si los hubiese, influencian el curso de la enfermedad. Sencillamente, aún no sabemos cuáles son las causas.
Otra área importante de las investigaciones del NICHD es la búsqueda de marcadores de la endometriosis. Estos marcadores son substancias hechas por o como respuesta a la endometriosis, que los profesionales de la salud pueden medir en la sangre o en la orina. Si se encontraran estos marcadores, los profesionales de la salud podrían diagnosticar la endometriosis haciéndoles exámenes de la sangre o de la orina a las mujeres, lo que podría reducir la necesidad de la cirugía.
¿Cómo sé si tengo endometriosis?
Actualmente, los profesionales de la salud utilizan varias pruebas para la endometriosis. A veces usan pruebas de imaginería para producir una “fotografía” del interior del cuerpo lo que les permite localizar áreas grandes de endometriosis, como nódulos o quistes. Las dos pruebas más comunes de imaginería son el ultrasonido o ecosonograma, una máquina que utiliza las ondas sonoras para hacer la “fotografía” y la resonancia magnética (MRI), una máquina que utiliza imanes y ondas de radio para hacer la “fotografía”.
La única manera de saber con seguridad si usted tiene endometriosis es mediante la cirugía. El tipo más común de cirugía es la laparoscopia. En este procedimiento, el cirujano infla levemente el abdomen con un gas inocuo.
Después de realizar una pequeña incisión en el abdomen, el cirujano utiliza un instrumento pequeño de observación con una luz, llamado un laparoscopio, para mirar los órganos reproductivos, los intestinos y otras superficies para ver si hay alguna endometriosis y hacer un diagnóstico basado en la apariencia característica de la endometriosis. Este diagnóstico se puede confirmar haciendo una biopsia, lo que involucra tomar una muestra pequeña de tejido para estudiarla bajo un microscopio.
Su profesional de la salud solamente hará una laparoscopia después de conocer su historia médica completa y de hacerle un examen físico completo, incluyendo un examen pélvico. Esta información, conjuntamente con los resultados de un ultrasonido o MRI, le ayudarán a usted y a su profesional de la salud a tomar decisiones más informadas sobre el tratamiento a seguir.
¿Por qué la endometriosis causa dolor?
Why endometriosis causes pain is the issue of many research. Because many women who have endometriosis feel pain during or related to their periods, some researchers are focusing their studies in the menstrual cycle to find the responses about pain.
Normally, if a woman is not pregnant, her endometrial tissue grows inside her uterus, decomposes in blood and tissue, and is detached as a flow or menstrual period. This cycle of growth and detachment occurs approximately every month.
Areas with endometriosis that grow outside the uterus also go through a similar cycle: grow, decompose in blood and tissue and are expelled once a month. But, because this tissue is not where it should be, it can not come out of the body in the same way that the women's menstrual flow normally does it. As part of this process, areas with endometriosis produce chemicals that can irritate close tissue and other chemicals that are known cause pain.
Over time, when going through this monthly cycle, areas with endometriosis can grow and become nodules or masses on the surface of the pelvic organs or can become cysts (sacs full of liquids) in the ovaries. Sometimes the chemicals produced by endometriosis can produce scars in the organs of the pelvic area or even cause them to come together when healing so that they seem a single large organ.
Is there any cure for endometriosis?
Currently we have no cure for endometriosis. Not even a hysterectomy or removal of the ovaries guarantees that the areas of endometriosis or the symptoms of endometriosis do not resort.
Is endometriosis the same as endometrial cancer?
Endometriosis is not the same as endometrial cancer. Remember that the word endometrium describes the tissue that is inside the uterus. Endometrial cancer is a type of cancer that affects the coating of the interior of the uterus, that is, the wall of the uterus. Endometriosis itself is not a form of cancer.
Does cancer endometriosis drive?
Current investigations have not shown that there is an association between endometriosis and endometrial, cervical, uterine or ovarian cancer. In very rare cases (less than 1 percent), endometriosis appears with a certain type of cancer called endometrioid cancer, but it has not been proven that endometriosis causes this cancer.
However, scientists still do not know what causes endometriosis or what their mechanisms are within the body. In addition, many women are never diagnosed with endometriosis, which makes it difficult to verify any loop between endometriosis and other diseases.
For this reason, women diagnosed with endometriosis must be especially attentive to changes in their body and must communicate these changes to their healthcare professional as soon as possible, to maintain their health.
Do the endometriosis ever disappear?
In most cases, the symptoms of endometriosis decrease after menopause because the growths are gradually reduced. However, in some women, that does not happen.
How to choose your gynecologist?
Consider these tips and follow those that fit more about your way of seeing things. Since you are sexually active you must attend the gynecologist to give you advice on contraceptive methods and make your annual reviews (Papanicolaou and Breast Exploration - and I teach you how to perform self-exploration).
Gender
How do you feel most comfortable, with a doctor or a doctor? It is a myth that gynecologists are more abrupt than gynecologists. Nor is it true that gynecologists see you as a woman, for them we are patients and do not impact the feminine anatomy. Choose the genre with which you feel more at ease.
Age
Do you prefer a young or older doctor? Here the advantages: the young doctor surely has a few years of having left college and is more updated on the subject. In addition, generally and due to the great competition of the field, it has more than one specialty, for example: gynecologist (that is the basic specialty of it), a specialist in climacterium (second specialty). On the other hand, the younger doctor has more medical experience. Evaluate which of the two cases has more value for you -Experience or fresh knowledge- and decide.
Cultural heritage
When you live in the United States it is very important that you consider this variable. Above all, if you already had some kind of contact with doctors in your country of origin. Here the doctors are not as warm as in Latin America, not only for their cultural origin but by fear of demands. It does not have to be Latin, even doctors of Asian, Indian or other context, can establish with you a relationship more similar to what you are accustomed.
In addition, doctors who are not Anglo-Saxon are more accustomed to common diseases of different ethnic groups. For example, in pediatrics, they know that Asians and Latinos are born with higher levels of bilirubin (they call them in English Joundice), and treat it with more naturalness. Now an example in the Gynecology area, Dr. Latino, knows that our community has a propensity to diabetes. So they closely monitor the sugar levels of pregnant women to avoid gestational diabetes.
Objective
What is your goal: preventive or reproductive health? It is very different when you still do not want to have children. Your relationship with your gynecologist is once a year. But if you already want to start having children or you are already pregnant is a relationship of at least once a month (at least at the beginning) and above all a relationship in which you are very vulnerable because as a pregnant woman sure you feel apprehension for well-being of the baby and your health. So it depends on the situation, effort and investment you should print on the gynecologist's research.
References
After having considered the above and decided what you expect from a gynecologist now look between your friends, well-known, co-workers or school and neighbors a positive reference, which satisfies you. Do not forget to ask the key questions: How is it in your deal? Is it punctual? How is your administrative team?, Is your nursing team friendly? If you plan to attend your pregnancies, the gynecologist attends the births? Who are your partners?
Do your inquiry well and choose the one that best suits you.And if something you do not like something, look for another.In the end, you will find one that fulfills your expectations.
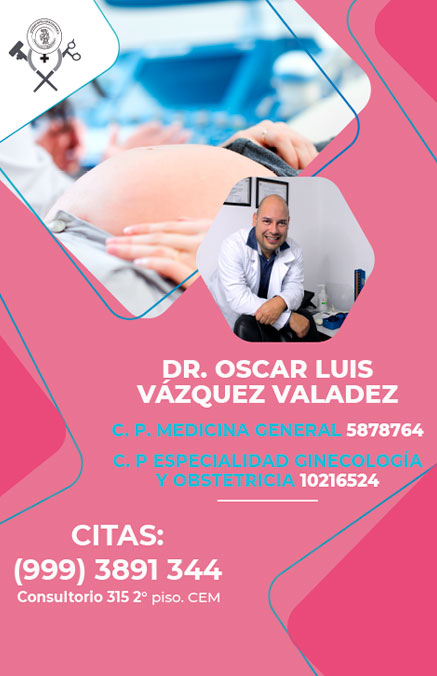
Find the best gynecologists in Merida
Do you want to be part of the Gynecologists community in Merida?
See more
Gynecologists consultations at Merida
Privacy Policy
The information herequis;Presented is the responsibility of the advertiser, Directory of Ginécologos in Merida IT DROPS from Any Claim or Problem With Any of the Advertisers.
Do you have any questions about Gynecologists in Merida?
Contact us